
Using DSM-IV, individuals with pathological hoarding behaviors could receive a diagnosis of obsessive-compulsive disorder (OCD), obsessive-compulsive personality disorder, anxiety disorder not otherwise specified or no diagnosis at all, since many severe cases of hoarding are not accompanied by obsessive or compulsive behavior. Hoarding disorder is included in DSM-5 because research shows that it is a distinct disorder with distinct treatments. While some people who hoard may not be particularly distressed by their behavior, their behavior can be distressing to other people, such as family members or landlords.
Symptoms of the disorder cause clinically significant distress or impairment in social, occupational or other important areas of functioning including maintaining an environment for self and/or others. They accumulate a large number of possessions that often fill up or clutter active living areas of the home or workplace to the extent that their intended use is no longer possible. For individuals who hoard, the quantity of their collected items sets them apart from people with normal collecting behaviors. The behavior usually has harmful effects - emotional, physical, social, financial, and even legal - for the person suffering from the disorder and family members. Hoarding disorder is characterized by the persistent difficulty discarding or parting with possessions, regardless of the value others may attribute to these possessions, according to the APA’s new criteria: After the DSM-5 OCD working group examined the research literature on hoarding, they found little support to suggest this was simply a variant of a personality disorder, or a component of another mental disorder. Hoarding disorder graduates from being listed as just one symptom of obsessive-compulsive personality disorder in the DSM-IV, to a full-blown diagnostic category in the DSM-5. Instead, it gets the new “absent/delusional beliefs” specifier. The delusional variant of body dysmorphic disorder (which identifies individuals who are completely convinced that their perceived defects or flaws are truly abnormal appearing) is no longer coded as both delusional disorder, somatic type, and body dysmorphic disorder. It was added to the DSM-5, according to the APA, to be consistent with data indicating the prevalence and importance of this symptom.Ī with muscle dysmorphia specifier has been added to reflect the research data, suggesting this is an important distinction to make for this disorder. This criterion describes repetitive behaviors or mental acts in response to preoccupations with perceived defects or flaws in physical appearance.
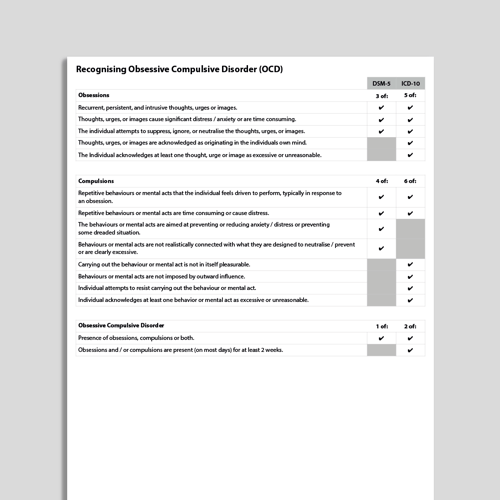
“These specifiers are intended to improve differential diagnosis by emphasizing that individuals with these two disorders may present with a range of insight into their disorder-related beliefs, including absent insight/delusional symptoms,” according to the APA.īody dysmorphic disorder in the DSM-5 remains largely unchanged from DSM-IV, but does include one additional criterion. These same insight specifiers have been included for body dysmorphic disorder and hoarding disorder as well. Absent insight/delusional obsessive-compulsive disorder beliefs (i.e., complete conviction that obsessive-compulsive disorder beliefs are true).

The old DSM-IV specifier with poor insight has been modified from being a black-and-white specifier, to allowing for some degrees on a spectrum of insight: Insight & Tic Specifiers for Obsessive-Compulsive and Related Disorders Disorders in this chapter include obsessive-compulsive disorder, body dysmorphic disorder and trichotillomania (hair-pulling disorder), as well as two new disorders: hoarding disorder and excoriation (skin-picking) disorder.


 0 kommentar(er)
0 kommentar(er)
